Four members of the PREDICT executive (Simon Craig, Stuart Dalziel, Elliot Long and Franz Babl) were invited to the EMCON2023 conference for the Society of Emergency Medicine in India in Hyderabad. PREDICT ran a one-day workshop aiming to support the beginning of multicentre research in India. This was well-received, and we plan to continue the collaboration with another visit in the first half of 2024.
Category: Newsletter
Congratulations to Associate Professor Amit Kochar
Congratulations to Amit Kochar from the Women’s and Children’s Hospital, Adelaide for being awarded the honorary title of Clinical Associate Professor (University of Adelaide). The award was based on research and educational achievements, service, and leadership in his field.
Project Snapshot – SONIC study
Study of Neck Injury Imaging in Children (SONIC): Improving the Diagnosis of Spinal Cord, Bone and Ligament Injuries
Many children sustain head and neck trauma during their lifetime. Significant neck injuries – to spinal cord, neck bones and connecting ligaments – can be identified by performing neck imaging with x-rays, or, if needed, computed tomography or magnetic resonance imaging. Yet, it is unclear which children should receive neck imaging in the emergency department (ED), especially in the context of increasing concerns about radiation-induced cancer in children and the discomfort and delays of immobilisation prior to imaging.
This study aims to:
- investigate the accuracy of existing neck injury clinical decision rules (CDRs) to detect neck injuries in children (external validation) of adult focussed CDRs and the newly developed paediatric PECARN CDR;
- derive and validate a new CDR for neck imaging in children (the SONIC CDR);
- assess the cost implications of different CDRs in children;
- investigate the epidemiology of cervical spine injuries in ANZ.
Study design:
Multicentre, prospective observational study.
Timeframe:
2020 – 2025
Sites: See link to SONIC project page.
Sample:
PREDICT ~30,000 (depending on prevalence of injuries), children aged <16 yrs with sustained or suspected blunt trauma with at least one of the following: Initiation of spinal precautions pre ED arrival, neck pain and/or considered at risk of CSI by any assessing clinician.
News:
Recruitment has commenced at all sites with over 7000 patients enrolled to date.
We have recruited approximately 100 patients to date with eligible cervical spine injuries (2/3 of the required number). These eligible patients for accuracy analysis are currently being reviewed by the study spinal surgeons.
Sites are doing an amazing job at recruitment and keeping our missed eligible patient rate at a minimum.
We project that study recruitment will need to continue throughout 2024 and potentially to early 2025 at some sites to ensure we reach the required number of positive injuries.
Project Snapshot -Triage tools for detecting cervical spine injury
Cochrane Review – Triage tools for detecting cervical spine injury in paediatric trauma patients
Co-ordinating PI:
Emma Tavender
Study Co-ordinator: N/A
Project aim/s:
To expand the scope and update the Cochrane review ‘ Triage tools for detecting cervical spine injury in paediatric trauma patients (updated search from 2017 to 3 June 2021) to determine the diagnostic accuracy of clinical decision rules (CDRs) or sets of clinical criteria used to evaluate for cervical spine injury (CSI) following blunt trauma in a paediatric population.
Study design:
Cochrane Diagnostic Accuracy Review.
Study types:
Diagnostic studies with cross-sectional or cohort designs (retrospective or prospective) and randomised controlled trials. We only included results from full reports. We excluded case-control studies and reports that evaluated predictor finding models because of the bias they might introduce. We preferred studies that evaluated the accuracy of CDRs in direct comparisons to each other, however, we did not exclude studies with indirect comparisons as we expected the number of studies with direct comparisons to be limited.
Index test:
Any CDR or set of clinical criteria that compared the diagnostic accuracy of the test for the target condition with the reference standard.
Reference test:
Computed tomography (CT), plain radiography (X-ray) or magnetic resonance imaging (MRI). We also included studies where the cervical spine was clinically cleared in the emergency department in low risk patients at the treating clinician’s discretion. We preferred to include studies where patients who did not receive imaging underwent either a medical record review or an additional follow up some time after discharge to ensure no CSIs were missed or other systems were used to ensure initially missed CSI were diagnosed. The imaging or clinical follow up should be undertaken within 72 hours of presentation to the ED.
Target condition:
Clinically-important cervical spine injury (CSI), defined as any fracture, dislocation, ligamentous injury or spinal cord injury (either detectable by diagnostic imaging or spinal cord injury without radiographic association) involving the cervical region and attaching ligamentous structures.
Current status:
Completed, accepted and currently being copy-edited.
Getting to know you – meet Katherine Cantos
Our “Getting to Know You” segment ensures PREDICT members are aware of new members, their interests and areas of expertise and where they are located.
This month we introduce Katherine Cantos from Monash Children’s Hospital.
“I work at Monash Children’s Hospital in Emergency, the Canopy ward and now with the paediatric ED research team! I’m very interested in research as I’d love to be a part of learning about and making improvements to the care we provide in hospital so that we can improve oucomes for unwell children all over the world. Every little bit counts and I’ve very much enjoyed getting on board with the research team to work with other nurses and doctors in our Emergency Department in a variety of different and interesting projects.”
Welcome to PREDICT Katherine!
New PREDICT publications
Congratulations to the following PREDICT authors:
Curran J, Wozney L, Tavender E, Wilson C, Ritchie KC, Wong H, Gallant A, Somerville M, Archambault PM, Cassidy C, Jabbour M, Mackay R, Plint AC “Implementing Electronic Discharge Communication Tools in Pediatric Emergency Departments: Multicountry, Cross-Sectional Readiness Survey of Nurses and Physicians”. JMIR Hum Factors 2023;10:e46379 doi: 10.2196/46379 PMID: 37819696.
Parr M, Wilson CL, Jones B, Crawford NW, Ferguson S, Ramesh S, Eapen N, Craig S, Hearps S, Babl FE. Emergency department presentations for chest complaints after mRNA COVID‐19 vaccinations in children and adolescents. Emergency Medicine Australasia. 2023-10-23. DOI: 10.1111/1742-6723.14327.
Getting to know you – meet Louise Mills
Our “Getting to Know You” segment ensures PREDICT members are aware of new members, their interests and areas of expertise and where they are located.
This month we introduce Louise Mills from Prince Charles Hospital, Brisbane.
“I work at The Prince Charles Hospital, Brisbane where we have separate General Adult and Children’s emergency departments. I work as both a Clinical Nurse in General ED and as a Nurse Researcher within both Emergency Departments. In my role as part of the research team I am responsible for recruitment and clinical data collection of studies currently underway and I also prepare information for the Site Specific Applications for future studies. I feel privileged to be actively involved in both locally and internationally recognised research, and to be able to contribute to the health and wellbeing of people of all ages and their families.”
Welcome to PREDICT Louise!
Project Snapshot – Head Injury Co-design
Co-designing discharge communication strategies for paediatric minor head injuries.
Co-ordinating PI:
Emma Tavender/Franz Babl
Study Co-ordinator ANZ
Emma Tavender/Cate Wilson
Study aim/s:
To improve discharge communication currently provided to children presenting to the ED with mild to moderate head injuries (concussion). Specifically, adolescents who have an increased risk of post-concussion symptoms (PCS).
Study design:
Mixed Methods: stepped co-design method to engage consumers (parents and youths) and clinicians in the development of head injury discharge communication strategies.
Primary outcome:
Co-designed discharge communication strategies for adolescents with mild to moderate head injuries (concussion) with parents, youths and clinicians.
Additional outcomes:
- Training materials that can be used for future co-design efforts
- Advancement in the science of implementation and contribution to future discharge communication strategy development for other common paediatric ED presentations.
Current status:
- Ethics received from RCH and Western Health.
- Recruited four parents, four clinicians and three youths to participate.
- Orientation/training session plus three meetings held.
- Priorities for improvement have been determined.
- List of priorities reduced to two key areas for improvement: Head injury: what to expect in the ED and Concussion discharge information.
- Prototype to address the two key priorities that have been developed and updated in response to new International Sports-related Concussion guidance (Amsterdam 2023)
- Plan to start usability testing end 2023/early 2024.
BREAKING NEWS – NHMRC Centre of Research Excellence grant application successful!
We are very excited to announce that we have received NHMRC (National Health and Medical Research Council) CRE funding ($2.5m) for the next 5 years which will support us to continue our PREDICT research plans.
The new CRE will continue to target conditions including sepsis and acute respiratory conditions like asthma, bronchiolitis and pneumonia. Additionally there will be a focus on improving family input at all stages of the trial design and execution and improved translation plus tracking of changes in care.
Over the next five years, the grant will also fund the creation of a family-facing smartphone app for families for certain high-risk conditions and an emergency department-focused implementation toolkit that can be adapted for hospitals across Australia and New Zealand.
The NHMRC funding will also develop Australia’s future workforce, training emerging leaders in emergency care through the creation of higher degree scholarships and postdoctoral opportunities. Through research and the implementation of best evidence, students and researchers within the CRE in Paediatric Emergency Medicine will be mentored across specialties and disciplines to become independent researchers who can improve the lives of all children who visit emergency departments.
The application was a massive collaborative effort from many people across many sites and thanks goes to all involved in this successful application.
We will discuss the CRE at the next PREDICT members meeting in November and look forward to an exciting and productive future for PREDICT!
Project Snapshot – BIPED
BI-PED Study
A Randomised Controlled Trial Comparing Epinephrine and Dexamethasone to Placebo in the Treatment of Infants with Bronchiolitis
Co-ordinating PI:
Amy Plint (Canada), Ed Oakley (Australia), Stuart Dalziel (New Zealand)
Study Co-ordinator ANZ
Sharon O’Brien
Study design:
International, multicentre, Phase 111, double-blind, randomised controlled trial
For further details about the study please see: https://www.predict.org.au/new-projects/bi-ped-study/
Current status:
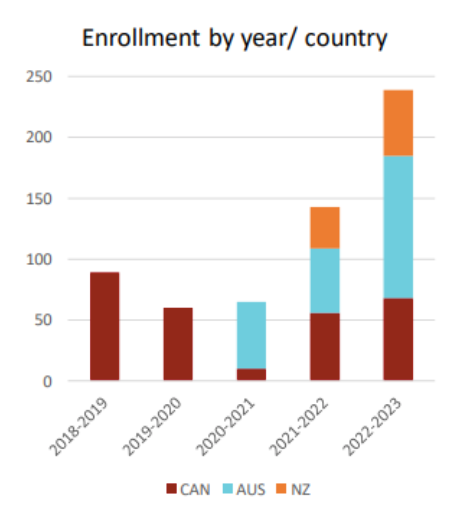
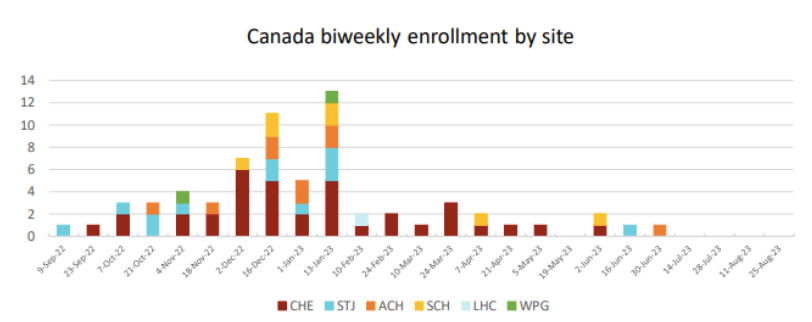
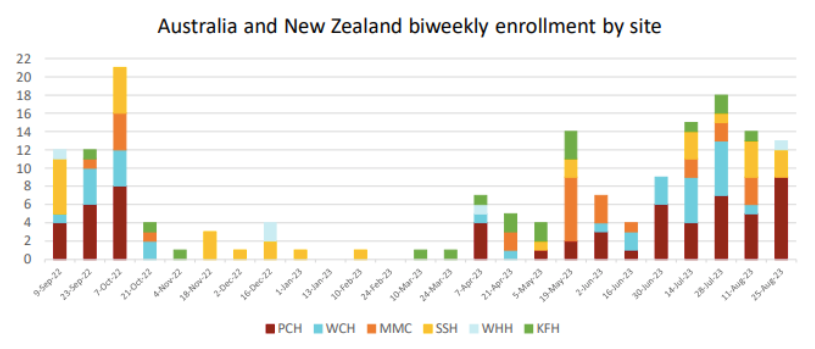
The research team are pleased to announce that the 5th season of the BIPED trial has been the most successful yet, reaching 598/864 participants recruited! The yearly recruitment was 28% of our total sample size; almost 100 more participants were enrolled in season 5 than were enrolled in season 4.
We have just over 30% (266) of our sample size left to recruit!
Please see below a number of charts which show study progress both locally and internationally.
| Country | Site | Total Recruitment | Season 5 recruiment |
|---|---|---|---|
| Canada | Children's Hospital of Eastern Ontario (CHE) | 142 | 36 |
| Canada | CHU Sainte Justine (STJ) | 47 | 12 |
| Canada | Alberta Children's Hospital (ACH) | 44 | 9 |
| Canada | Stollery Children's Hospital (SCH) | 21 | 7 |
| Canada | Children's Hospital of Winnepeg (WPG) | 18 | 3 |
| Canada | London Health Sciences (LHC) | 11 | 1 |
| Australia | Perth Children's Hospital (PCH) | 143 | 60 |
| Australia | Women's and Children's Hospital (WCH) | 48 | 31 |
| Australia | Monash Medical Center (MMC) | 36 | 26 |
| New Zealand | Starship Children's Hospital (SSH) | 52 | 33 |
| New Zealand | Kidz First Middlemore Hospital (KFH) | 21 | 17 |
| New Zealand | Waikato Hospital) (WHH) | 15 | 5 |
| TOTAL | 598 | 239 |